Connect With Us
Blog

Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Cracked Heels and Their Effects
 Cracked heels, medically known as keratoderma, is a condition where the skin on the heels becomes thick, dry, and eventually splits. This often painful issue arises from prolonged pressure on the feet, leading to hard, callused skin that can fissure. Causes include standing for long periods, wearing open-backed shoes, and exposure to dry, cold weather. Medical conditions like diabetes and hypothyroidism also contribute by causing excessively dry skin. Excessive weight increases pressure on the heel pads, further worsening the problem. Preventing keratoderma involves regular moisturizing, wearing supportive, closed-back footwear, and avoiding prolonged standing on hard surfaces. Proper foot care routines, including gentle exfoliation and hydration, are essential to maintain soft, healthy skin and prevent the discomfort associated with cracked heels. This condition can be painful. If this applies to you, it is suggested that you visit a podiatrist who can effectively treat cracked heels, which often includes prescribed medication.
Cracked heels, medically known as keratoderma, is a condition where the skin on the heels becomes thick, dry, and eventually splits. This often painful issue arises from prolonged pressure on the feet, leading to hard, callused skin that can fissure. Causes include standing for long periods, wearing open-backed shoes, and exposure to dry, cold weather. Medical conditions like diabetes and hypothyroidism also contribute by causing excessively dry skin. Excessive weight increases pressure on the heel pads, further worsening the problem. Preventing keratoderma involves regular moisturizing, wearing supportive, closed-back footwear, and avoiding prolonged standing on hard surfaces. Proper foot care routines, including gentle exfoliation and hydration, are essential to maintain soft, healthy skin and prevent the discomfort associated with cracked heels. This condition can be painful. If this applies to you, it is suggested that you visit a podiatrist who can effectively treat cracked heels, which often includes prescribed medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
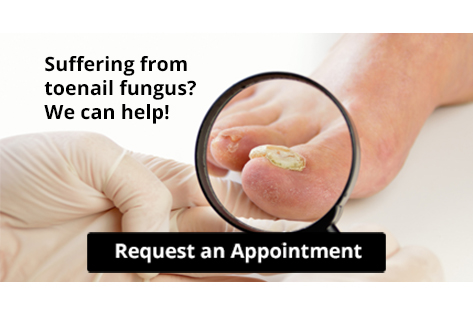
Understanding Toenail Fungus

Toenail fungus, or onychomycosis, is a common condition where a fungal infection affects the toenails, causing them to become discolored, thickened, and brittle. This happens when fungi, including dermatophytes, yeasts, or molds, infiltrate the nail bed through cracks or cuts. Warm, moist environments, such as sweaty shoes or public showers, are ideal for fungal growth, making these areas common sources of infection. Poor foot hygiene, compromised immune systems, and conditions like diabetes can increase the risk. Preventing toenail fungus involves keeping feet clean and dry, wearing breathable footwear, and avoiding walking barefoot in communal areas. Regularly trimming nails and avoiding shared nail care tools can also help to reduce the risk of infection. Toenail fungus can be uncomfortable and unsightly. If you have developed this condition, it is suggested that you visit a podiatrist who can offer you prescribed medication for a full recovery.
For more information about treatment, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Quality of Life and Heel Pain
 Plantar heel pain, often caused by plantar fasciitis, can significantly impact quality of life. This condition occurs when the thick band of tissue running along the bottom of the foot becomes inflamed, typically due to overuse or strain. The resulting pain can make walking and standing difficult, limiting daily activities and reducing overall mobility. Factors such as wearing poor footwear, obesity, and prolonged standing contribute to this issue. To alleviate plantar heel pain, several measures can be taken. Wearing supportive shoes with proper arch support and cushioning is vital. Stretching exercises for the calf and foot can help relieve tension in the plantar fascia. Taking pain relievers can reduce inflammation and discomfort. In severe cases, custom orthotics may be necessary. If you have persistent heel pain, it is suggested that you schedule an appointment with a podiatrist for effective treatment and long-term relief.
Plantar heel pain, often caused by plantar fasciitis, can significantly impact quality of life. This condition occurs when the thick band of tissue running along the bottom of the foot becomes inflamed, typically due to overuse or strain. The resulting pain can make walking and standing difficult, limiting daily activities and reducing overall mobility. Factors such as wearing poor footwear, obesity, and prolonged standing contribute to this issue. To alleviate plantar heel pain, several measures can be taken. Wearing supportive shoes with proper arch support and cushioning is vital. Stretching exercises for the calf and foot can help relieve tension in the plantar fascia. Taking pain relievers can reduce inflammation and discomfort. In severe cases, custom orthotics may be necessary. If you have persistent heel pain, it is suggested that you schedule an appointment with a podiatrist for effective treatment and long-term relief.
Many people suffer from bouts of heel pain. For more information, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Gout and Its Impact on Women
 Gout, a form of arthritis caused by the buildup of uric acid crystals in the joints, affects both men and women, though it is more prevalent in men. However, women are increasingly affected, especially after menopause. Before menopause, estrogen helps to lower uric acid levels, providing a protective effect. After menopause, the decline in estrogen levels leads to higher uric acid levels, increasing the risk of gout. Women with gout often experience symptoms in different joints compared to men, with a higher likelihood of affecting the knees and wrists. Additionally, women may face a delayed diagnosis, as gout is traditionally associated with men. Understanding the gender differences in gout can lead to better awareness and treatment options for women, ensuring timely management and improved quality of life. Gout generally affects the joints and the big toe and can produce a significant amount of pain and discomfort. If you have this type of foot pain, it is strongly suggested that you visit a podiatrist who can help you to manage this condition.
Gout, a form of arthritis caused by the buildup of uric acid crystals in the joints, affects both men and women, though it is more prevalent in men. However, women are increasingly affected, especially after menopause. Before menopause, estrogen helps to lower uric acid levels, providing a protective effect. After menopause, the decline in estrogen levels leads to higher uric acid levels, increasing the risk of gout. Women with gout often experience symptoms in different joints compared to men, with a higher likelihood of affecting the knees and wrists. Additionally, women may face a delayed diagnosis, as gout is traditionally associated with men. Understanding the gender differences in gout can lead to better awareness and treatment options for women, ensuring timely management and improved quality of life. Gout generally affects the joints and the big toe and can produce a significant amount of pain and discomfort. If you have this type of foot pain, it is strongly suggested that you visit a podiatrist who can help you to manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.