Connect With Us
Blog

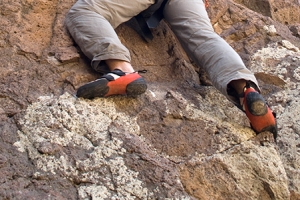
How Shoes Can Cause Rock Climbing Injuries
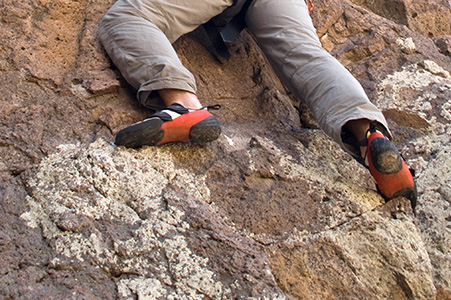
Foot injuries from rock climbing are more common than many people think, especially during falls or from wearing tight climbing shoes. Falls can lead to bruises, sprains, or broken bones in the heel or ankle, which may require surgery to heal properly. However, repeated impact and pressure from tight shoes can also cause long-term problems. These include pain in the toes, thickened skin, and blood under the toenails. Many climbers wear shoes that are too small in order to get a better grip, but this can change how the foot moves and put too much pressure on certain areas. Over time, this can lead to chronic foot pain and deformities that may limit movement or cause discomfort even when not climbing. Changes in toe shape, such as bunions, or stiffness in the big toe joint may also develop. A podiatrist can diagnose climbing-related foot and ankle injuries, help manage pain, and recommend the best medical treatment, which may include surgery if needed. If you have injured your foot while rock climbing, whether indoors or outside, it is suggested that you make an appointment with a podiatrist for treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
What Is a Plantar Fibroma?

A plantar fibroma is a benign growth that forms within the plantar fascia, a thick band of tissue along the bottom of the foot. This firm lump is usually located in the arch and may gradually increase in size. While it is noncancerous, a plantar fibroma can cause discomfort, especially while walking or standing for extended periods. Symptoms often include a noticeable lump, aching pain, or a sensation of pressure when wearing shoes. The exact cause of plantar fibromas is not fully understood, but factors such as genetic predisposition, trauma to the foot, or underlying medical conditions may contribute. Early identification and appropriate care can help manage uncomfortable symptoms. If you have a lump on the sole of your foot, it is suggested that you confer with a podiatrist who can offer you relief and management tips.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Plantar Fibroma
A plantar fibroma is a knot in the arch of the foot. It can cause pain when repeated pressure is applied by walking barefoot or wearing tight shoes. While plantar fibromas can appear in anyone, men who are middle-aged or older are said to be more susceptible. The main symptom of a plantar fibroma is a firm lump on the arch of the foot. If there is pain, it can be intensified by putting pressure on the nodule. The lump can stay one size or grow larger. You may have one or more fibromas in the feet and there tends to be a high incidence of recurring plantar fibromas. Generally, a plantar fibroma can be treated without surgery. Treatment might include steroid injections to help shrink the lump, orthotics to help redistribute weight away from the nodule, plantar fascia stretching, or physical therapy to help use anti-inflammatory medication on the lump. If a lump grows larger or more painful, a podiatrist can be consulted to confirm the diagnosis. The doctor will palpate the lump and this may cause pain that can be felt all the way to the toes. An X-ray, MRI, or biopsy might be done if further evaluation is necessary. A lump in the arch of the foot might be something other than a plantar fibroma, such as cysts, nerve or fatty tumors, swollen tendons, or an infection in the foot. It is important to see a podiatrist for proper diagnosis and treatment of plantar fibromas.
Dealing With Diabetic Neuropathy

Diabetic neuropathy is a complication of diabetes that affects the nerves in the feet and legs, leading to numbness, tingling, burning, or sharp pain. As nerve damage progresses, it can reduce sensation, making it difficult to feel cuts, blisters, or sores. This can lead to infections, ulcers, or deformities like hammertoe, where the toes become bent or misaligned. The primary cause of diabetic neuropathy is high blood sugar levels over time, which can damage both blood vessels and nerves. Poor circulation combined with nerve damage increases the risk of developing foot ulcers and deformities, which may become severe if left untreated. A podiatrist can help manage diabetic neuropathy by providing regular foot exams, treating ulcers, and recommending special footwear or custom orthotics to prevent further damage. They can also assist with managing hammertoe and other foot deformities. If you are dealing with diabetic neuropathy, it is suggested that you make an appointment with a podiatrist.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Bunions and Surgical Treatment Options

A bunion is a bony bump that forms at the base of the big toe due to misalignment of the foot’s bones. This condition causes the tip of the big toe to shift toward the smaller toes, leading to discomfort, swelling, and difficulty walking. When conservative treatments are not effective, bunion surgery may be necessary to relieve pain and correct the deformity. An osteotomy involves cutting and realigning the bone to restore proper positioning. An exostectomy focuses on removing the bony prominence without realigning the joint. An arthrodesis fuses the affected joint to eliminate movement and pain, while a resection arthroplasty removes a portion of the bone to create more space within the joint. Each procedure is chosen based on the severity of the bunion and the patient’s individual needs to improve function and comfort. If you have a bunion that is painful, it is strongly suggested that you consult a podiatrist who can determine if surgery is right for you, and which type you would most benefit from.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
The Possible Causes and Treatments of Plantar Fasciitis

The plantar fascia is a long, thick band of tissue that spans from the heel bone along the bottom of the foot to the toes. The plantar fascia supports the bottom of the feet and toes during walking, running, and jumping. The plantar fascia can become overly stressed or even tear or rupture from overuse or injury, causing pain and inflammation which causes plantar fasciitis. Being obese, standing or working on your feet for prolonged periods of time, or having flat feet or high arches can all contribute to this condition. Additionally, engaging in activities that involve dancing, marching or running can also contribute to, or possibly worsen the symptoms of plantar fasciitis. Wearing certain footwear can also put you at an increased risk of developing this condition such as high heels, flip flops, worn out shoes, or other types of footwear with inadequate support. A podiatrist will use a variety of treatment protocols to treat plantar fasciitis depending upon the severity of the condition and how long the patient has been suffering from it. If you have this kind of foot pain, it is suggested you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment plan.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.